Author: Dr Anand Senthi
8/7/23
Procedural sedation often requires the use of drugs (e.g. propofol) that can produce periods of apnoea, particular when used for procedures that require deeper levels of sedation (e.g. dislocated joints and fractures). If properly prepared for and managed it should essentially never cause an issue. The following Approach to Apnoea assumes the use of other suggested elements of the partner article, Approach to Procedural Sedation, including but not limited to the use of CO2 monitoring as well as nasal prong oxygen (running at only 3L/min) placed under the main pre-oxygenation device.
Stepwise Approach to Apnoea1
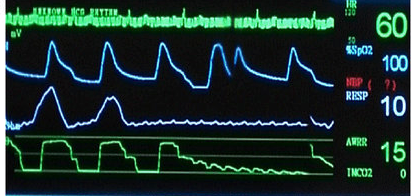
1. If you lose your CO2 trace = your apnoea alarm has gone off! This means you either have apnoea or airway obstruction (or both)
2. Open the airway (e.g. jaw thrust, head tilt).
- If CO2 returns, the problem was airway obstruction which you have now fixed.
- If CO2 does not return = apnoea confirmed2.
3. Stimulate the patient.
- Initially applying the bilateral Larson’s manoeuvre simultaneously with jaw thrust is quite stimulating. Other stimulation can be added (e.g sternal rub) but generally the best stimulation is to immediately commence the procedure (e.g. fracture reduction, cardioversion) if it has not yet been performed.
4. If apnoea persists, then perform Apnoeic Oxygenation
- Turn up the nasal prongs to 15/min while maintaining the airway (e.g jaw thrust)
- Assuming healthy lungs, this will generally provide a long period of safe apnoea. Combined with other essential aspects of the Approach to Procedural Sedation (including patient selection and careful drug selection/dosing) this should almost universally prevent desaturation.
- This will also prevent you engaging the traditional knee-jerk response of immediately using a Bag-Valve-Mask (BVM) ventilator which will likely inflate the stomach and increase your risk of aspiration.
- The only downside is that this will often wash out your CO2 trace so you will need to detect the resolution of apnoea by clinical assessment e.g. detecting chest/abdominal movement. Note that the primary purpose of the C02 alarm is to alert you to the onset of apnoea (before you would typically realise based on clinical assessment alone). Now that the “CO2 alarm” has gone off, it’s ongoing utility is minimal and outweighed by the benefit of continuing to oxygenate the patient, avoiding desaturation and unnecessary use of the BVM.
- Apnoeic oxygenation was traditionally popularised and advocated for the apnoea associated with intubation by Weingart (2010) & together with Levitan (2012). This Stepwise Approach to Apnoea instead applies it to the apnoea associated with procedural sedation using a strategically altered timing of commencement. Unlike intubation where it is started prior to the procedure, here that is avoided to prevent the loss of the “CO2 apnoea alarm” and is hence commenced only after apnoea resistant to stimulation is confirmed.
Notes
1) This approach above is based on a combination of related evidence and specialist opinion. However this specific approach has not been validated head to head against, for example, the early use of a BVM for apnoea. As a personal anecdote using this approach, the author has not had a patient experience a single episode of desaturation or required the use of a BVM during procedural sedation in almost a decade. Of course, an anecdotal case series is only worth so much but is shared with the ED community now to encourage feedback, comments, alternatives and other experiences in the Comments below.
2) Another cause of the loss of CO2 trace that should be considered is equipment failure. The above two options are a simplification that assumes the trace was working perfectly and was lost rapidly in expected temporal relation to a dose of sedative. Total laryngospasm is another rare cause of loss of CO2 trace. However this would usually first start as partial laryngospasm with stridor, paradoxical breathing, tracheal tug with some CO2 trace preserved. The bilateral Larson’s manoeuvre discussed above is also the first step in managing laryngospasm.
See also the Approach to Procedural Sedation for other key information provided to maximise the safety of procedural sedation.