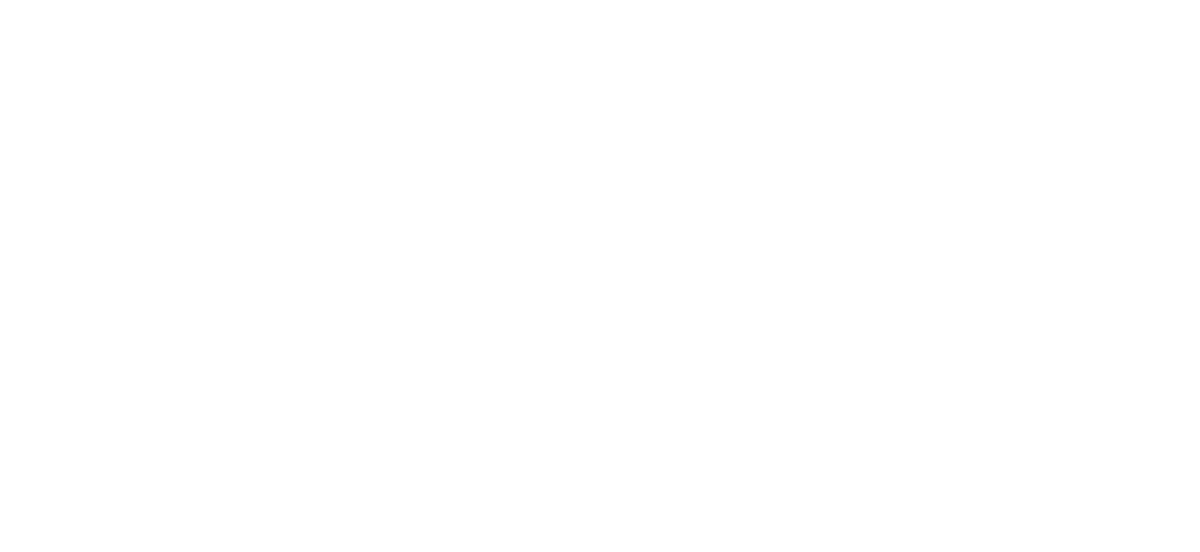
Basic Life Support (BLS) is the approach to the unconscious/collapsed patient that can be taught to all people, medical and non-medical.
It follows the well known DRSABCD approach.
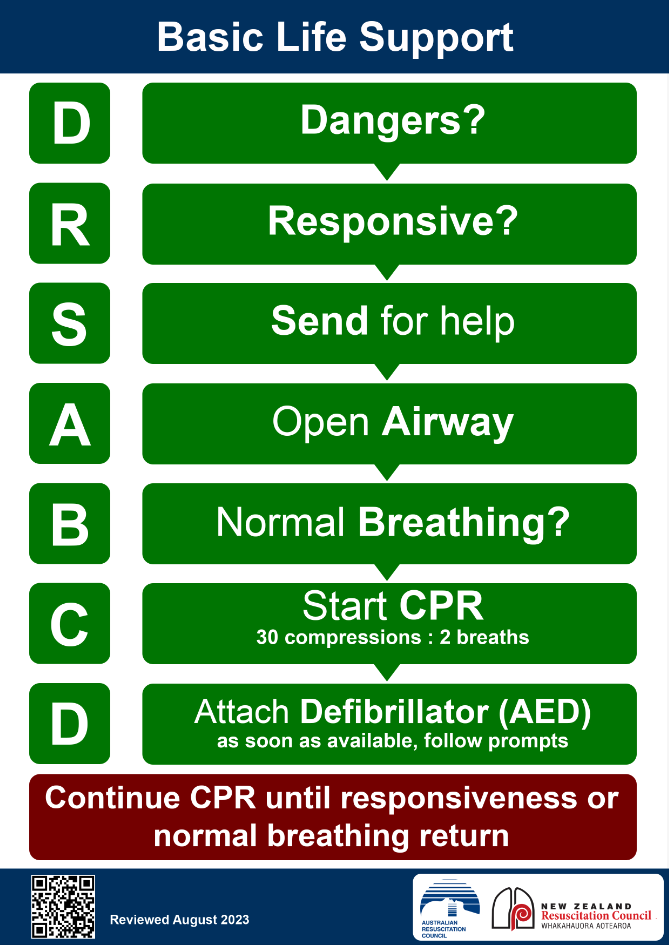
Advanced Life Support (ALS), also known in other countries as Advanced Cardiac Life Support (ACLS), is intended for clinical staff only (mainly doctors and nurses) and builds on BLS by adding a few extra considerations regarding how to treat other reversible causes. Notably it adds in certain drugs (adrenaline and amiodarone) and a list of 4 H’s and 4 Ts to denote the additional reversible causes.
As a Specialist Emergency Physician and ALS course instructor I find learners are often focused on minutia within ALS (in part due to the way the course is structured and assessed) without maintaining a “big picture” approach to what they are trying to achieve.
To refocus on the the true purpose and essence of ALS (and BLS for that matter), simply follow this phrase:
“Buy time until someone fixes something”
“Buy Time…”
Buying Time, means buying time for the brain, by providing high quality CPR in 2 ways:
- 1) Perform high quality cardiac compressions for the maximum time
- Commence straight away after rapidly confirming cardiac arrest (“look, listen and feel” for a maximum 10 seconds)
- High quality technique: compress the lower half of the sternum, 1/3 of the depth of the chest, at a rate of 100-120 bpm
- Absolutely minimise interruptions by a well trained team practising the “Defib Dance” – a series of drilled steps that minimise the pause in compressions while charging a defib, interpreting a rhythm and delivering a shock or dumping the charge is performed in sequence.
- 2) Provide the occasional breath of maximum oxygen
- Ventilation – Provide the occasional breath:
- Oxygen is critical, but the arrested patient does not need too many breaths
- The ratio is 30 compressions to 2 breaths (30:2).
- This ratio delivering only occasional breaths is designed to minimise interruptions to compressions.
- In fact in cases of sudden cardiac arrest (where hypoxia is unlikely the cause of arrest), in the first few minutes a single rescuer can provide compression only CPR as there is sufficient oxygen already in the blood.
- Oxygenation – Provide maximum oxygen by:
- Connecting the ventilating device to 100% oxygen
- The insertion of an advanced airway device such as the iGel (or ETT)
- This not only simplifies ventilation technique (as it is easier than mask ventilation) and thus maximises oxygen delivery but importantly allows the ventilation to occur asynchronously to cardiac compressions.
- This in turns helps provide compressions for the maximum time as there no longer needs to be a compression pause to deliver breaths
- With 100% oxygen a low asynchronous ventilation rate of 10 breaths/min is more than adequate.
- Ventilation – Provide the occasional breath:
“…Someone”
“Someone” simply means “not you” i.e. send for help at the start! You will rarely be able to save a life by yourself.
“…Fixes Something”
This is the primary target of ALS – if you don’t fix something, a patient lacking a pulse will not regain one.
The simplest thing you can fix is a shockable rhythm (VF or pulseless VT) which is why both BLS and ALS have their primary focus on sending for help, in part to obtain and attach a defibrillator as quickly as possible and perform a rhythm check (the S and 2nd D in DRSABCD). This is also the reason why shockable arrests have a substantially higher survival rate than non-shockable arrests, simply because there is something quick and easy to fix.
If you are unable to fix a shockable rhythm through early defibrillation or this is a non shockable rhythm, then you must rapidly fix something else. This leads to the classic list of reversible causes – the 4 H’s and 4 T’s of ALS.
- H1 = Hypoxia
- H2 = Hypovolaemia = includes both true hypovolaemia and relative hypovolaemia (ie. distributive hypovolaemia through widespread vasodilation)
- H3 = High or low electrolytes & metabolic disorders (often recited as “hyper/hypokalaemia etc …”)
- H4 = Hypothermia or hyperthermia
- T1 = Tension pneumothorax
- T2 = Tamponade
- T3 = Thrombosis (PE & Coronary)
- T4 = Toxins
While occasional candidates learning ALS can reliably remember this full list of 8 items, experience suggests many struggle to do so during their ALS courses, let alone years later in real clinical practice. With that in mind, it is important to have the ALS algorithm as shown here, available in critical care areas (e.g. on the walls of resus cubicles) and also on resuscitation trolleys in wards.
As a complementary approach to trying to remember an unfamiliar list of 8 items, considering that cardiac arrest is something most clinical staff rarely come across, it can be useful to view arrest as just a severe version of shock. Shock is far more commonly encountered by clinical staff, especially those working in hospitals, and conceptualising arrest in this way can be of dual educational and retention value. Shock is typically categorised in 4 groups provided by the acronym CHOD:
- C – Cardiogenic
- H – Hypovolaemic
- O – Obstructive
- D – Distributive
By viewing cardiac arrest as the extreme end of the shock spectrum, CHOD offers a higher-order mental model into which the 4 H’s and 4 T’s neatly fit. Some learners may find it easier to recall this short list of only 4 types of shock then consider the 4 H’s and Ts as merely subsets of this. Ideally learning both the list of 4 H’s and T’s and their place in the CHOD shock classification of causes may be complementary for memory retention value.
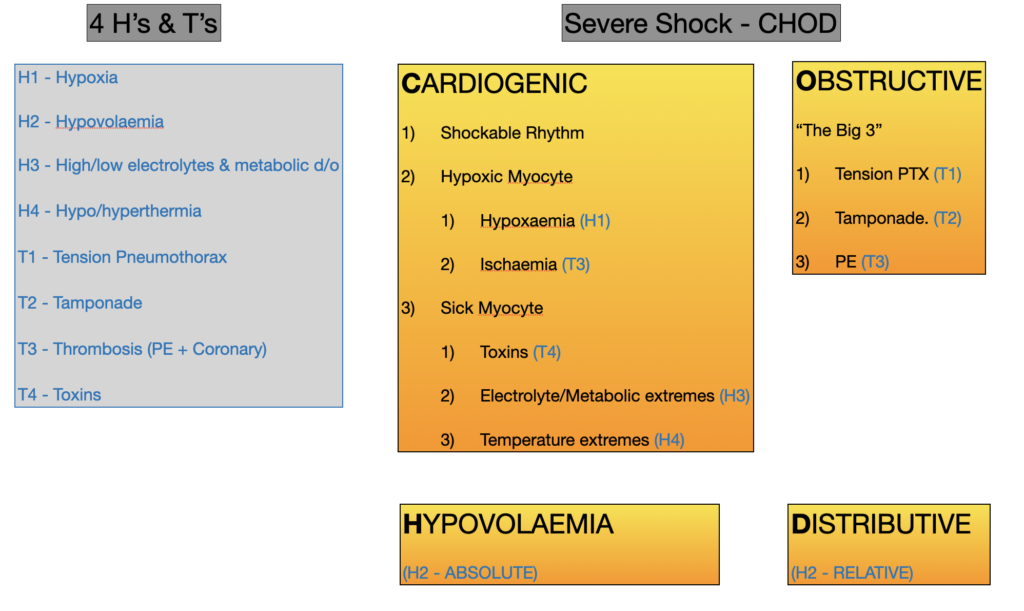
- C – Cardiogenic
- Shockable Rhythm
- Treatment –> Defibrillate –> refractory? –> Add Amiodarone (+ Double Sequential Defibrillation – not yet taught in ALS courses)
- Hypoxic Myocytes due to
- Hypoxaemia (H1)
- Treatment – Maximum Oxygen
- Ischaemia (T3 – Thrombosis – coronary)
- Treatment – Thrombolysis
- Hypoxaemia (H1)
- Sick Myocytes due to:
- 1) Toxins (T4 – Toxins)
- 2) Electrolytes/Metabolic extremes (H3 – High or low electrolytes & metabolic disorders)
- 3) Temperature extremes (H4 – Hyper/hypothermia)
- Treatment – correct and give antidotes
- Shockable Rhythm
-
- HINT – these causes can be remembered simply as 3 x Cardiogenic causes, with sequentially 1, 2 & 3 sub-set causes/treatments
- 1) Shockable Rhythm
- 2) Hypoxic Myocytes –> (1 – Hypoxaemia 2 – Ischaemia)
- 3) Sick Myocytes –> (1 – Tox 2 – Electrolyte/Metabolic, 3 – Temperature)
- HINT – these causes can be remembered simply as 3 x Cardiogenic causes, with sequentially 1, 2 & 3 sub-set causes/treatments
- Hypovolaemia (H2 – Hypovolaemia (true))
- Fluid or blood loss
- Treatment – IV fluid and/or blood
- Obstructive
- The big 3 – Tension PTX (T1), Cardiac Tamponade (T2), Pulmonary Embolus (T3)
- Treatment is as per cause:
- Tension PTX – needle thoracostomy, finger thoracostomy
- Tamponade – pericardiocentesis
- PE – thrombolysis
- Distributive (H2 – Hypovolaemia (relative))
- e.g. due to sepsis, anaphylaxis, neurogenic causes
- Treatment – IV adrenaline + IV fluids
Summary
This simple phrase“Buy time until someone fixes something” captures the essence of ALS. Breaking this phrase into its components while conceptualising what can be fixed (the 4 Hs and 4Ts) as merely treating severe shock (CHOD) can be useful complementary mental strategies to the traditional approach provided for teaching, learning and most importantly retaining and enacting the key components of ALS.